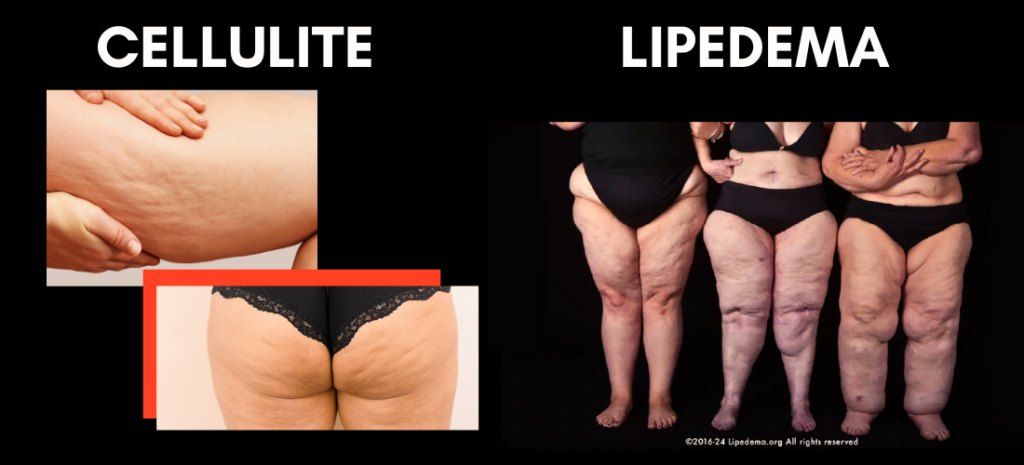
Cellulite or Lipedema? Let’s Figure It Out Together
Think all lumps and bumps are just cellulite? Many women go years without realizing they have lipedema, a condition needing a different approach. Knowing the difference can get you the right care—and feeling better, faster. Ever catch yourself staring at your legs, wondering why they look bumpy or feel off? You’re not alone—we hear it all the time at Body Lab Studio: “What’s going on with my skin?” Over coffee, let’s sort it out: cellulite treatment or lipedema support? We’ve got the science and solutions to help you feel your best.
What’s Cellulite All About?
Spot that “orange peel” texture on your thighs or hips? That’s cellulite, and it’s incredibly common—up to 90% of women see it at some point. It’s just fat nudging against your skin’s connective tissue, forming those painless dimples. Hormones, genetics, or aging skin elasticity play a part—it’s not a health concern, just a cosmetic one. We often hear, “Can I smooth this out?” At Body Lab Studio, our LPG Endermologie boosts circulation to soften that texture, helping you feel confident in your skin.
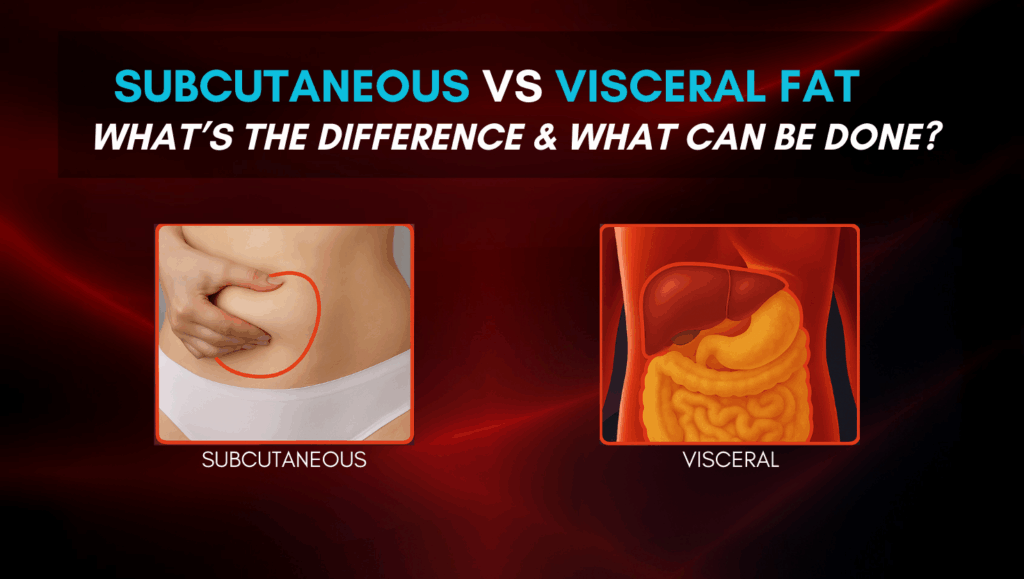
What’s Lipedema, Then?
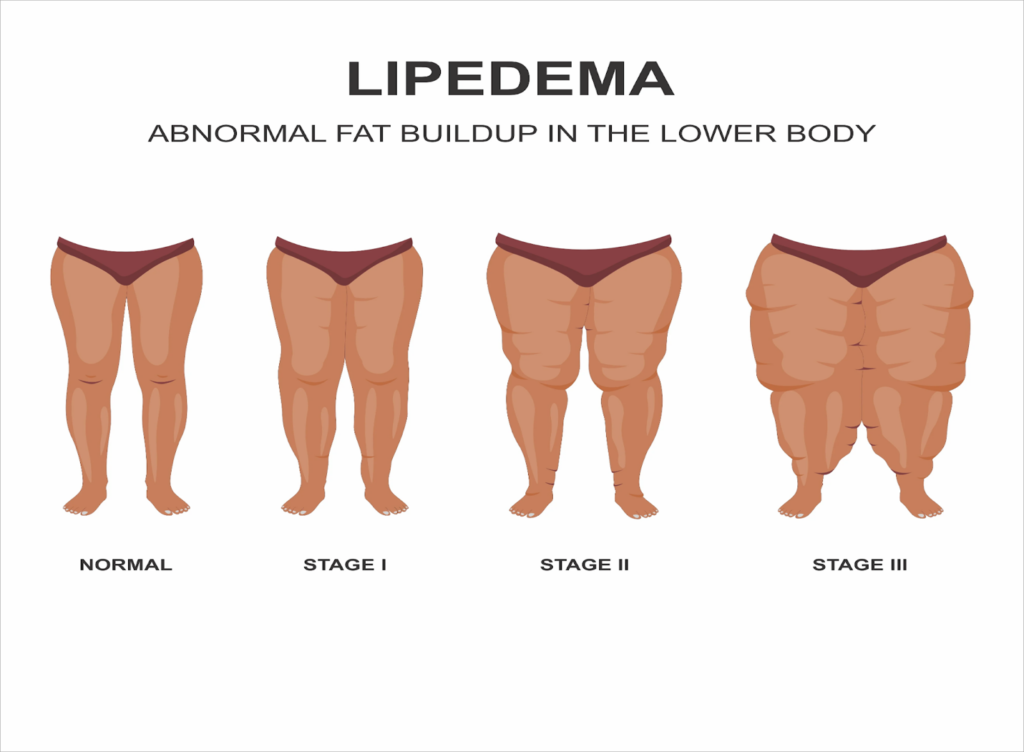
Unlike cellulite, lipedema isn’t just a surface-level change—it’s a chronic condition affecting about 11% of women. It leads to disproportionate fat buildup in the legs, often misdiagnosed as weight gain. Picture your legs feeling heavy, tender, or swollen—not just looking textured. It’s painful, bruises easily, and resists diet or exercise. A 2015 study in JAMA Internal Medicine tied heat therapy to better circulation, inspiring our infrared therapy to ease lipedema symptoms. If this sounds like you, we’re here with answers.Read more here

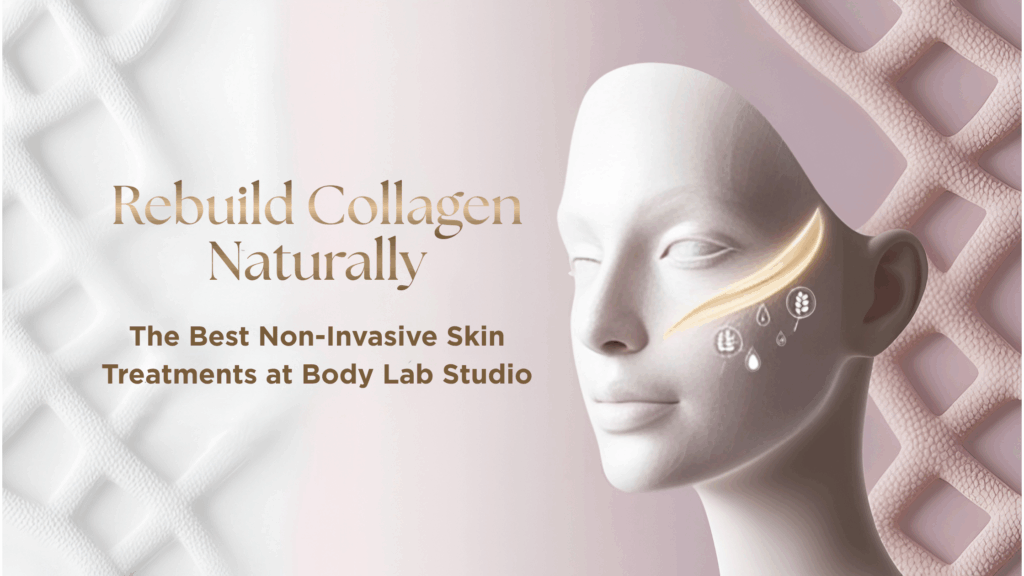
Cellulite vs. Lipedema: Quick Comparison
We hear it a lot: “I thought it was just cellulite!” This chart can guide you—let’s check it out for yourself next.
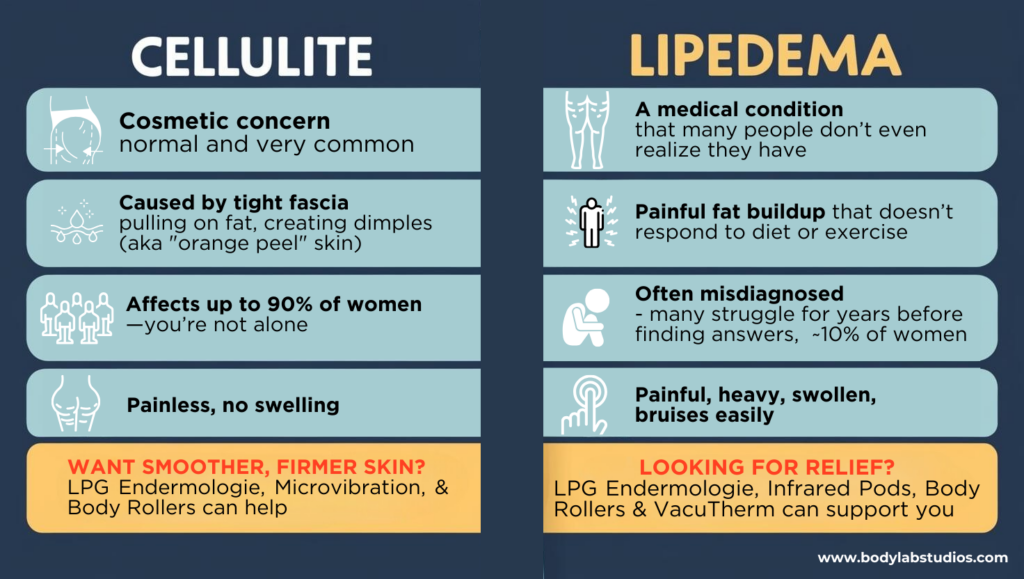
How to Tell the Difference
Not sure what’s going on? A simple self-check can offer clues—try this: Press on the area. If it feels tender, sore, or bruises easily, it might be lipedema. If it’s smooth and painless, it’s likely cellulite. Still wondering? Cellulite stays skin-deep, while lipedema brings that heavy, spongy feel—often in both legs. We get it—sorting this can feel tricky, but pinpointing it opens the door to feeling better. Ready to see how we can help?
How Body Lab Studio Can Help
Here’s where we step in with solutions. For cellulite, our LPG Endermologie massage smooths texture by boosting circulation—clients love that refreshed look. For lipedema, our infrared therapy helps promote lymphatic drainage, improving circulation to reduce swelling and discomfort. More movement, less fluid buildup, and relief you can feel—our Wellness Pods and Power Treadmill make it happen. Backed by science—like the Finnish Sauna Study—these aren’t cures, but powerful boosts. Most see a lift in weeks with regular sessions, and we’ll tailor it to you—cellulite reduction or lipedema relief, we’ve got your back

Tired of Guessing? Let’s Create Your Plan
Imagine sipping that last coffee, picturing legs that feel lighter, smoother, and truly yours—whether it’s tackling cellulite treatment or easing lipedema symptoms. Why keep wondering? Let’s create a plan that works for your body. Book your consultation today with Body Lab Studio and take the first step to feeling your best—click here to get started now!
REFERENCE
- Güleç, A. T. (2009). Treatment of cellulite with LPG endermologie. International Journal of Dermatology, 48(3), 265-270.
This study evaluated the efficacy of LPG endermologie in treating cellulite. Thirty-three women underwent 15 sessions, resulting in significant circumference reduction at all measured body sites. However, only 15% showed improved cellulite appearance.
pubmed.ncbi.nlm.nih.gov - Kutlubay, Z., Songur, A., Engin, B., Khatib, R., & Serdaroğlu, S. (2013). An alternative treatment modality for cellulite: LPG endermologie. Journal of Cosmetic and Laser Therapy, 15(5), 266-270.
In this study, 118 women received LPG endermologie treatments twice weekly for at least 15 sessions. Results showed a significant mean body circumference reduction of 2.9 cm per site, with 99% of participants experiencing loss in body measurements.
researchgate.net - Avram, M. M. (2004). Cellulite: a review of its physiology and treatment. Journal of Cosmetic and Laser Therapy, 6(4), 181-185.
This review discusses the physiology of cellulite and various treatment modalities, providing a comprehensive understanding of its causes and potential interventions. - Wold, L. E., Hines, E. A., & Allen, E. V. (1951). Lipedema of the legs: a syndrome characterized by fat legs and edema. Proceedings of the Staff Meetings of the Mayo Clinic, 26(7), 221-230.
This seminal paper first described lipedema, differentiating it from other conditions like obesity and lymphedema, and highlighting its unique clinical features. - Herbst, K. L. (2012). Lipedema: clinical and research perspectives. Obesity Surgery, 22(4), 521-523.
This article provides insights into the clinical presentation of lipedema, its progression, and challenges in diagnosis and treatment, emphasizing the need for increased awareness among healthcare providers.